author: Kevin Curran PhD
updated: 3-11-2020
Gene editing enters into human clinical trials
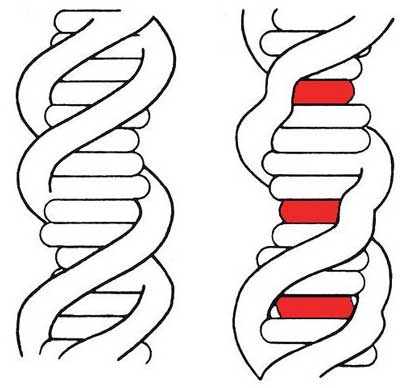
Gene editing technology allows scientists to change the DNA of an organism. This technology, also known as genome editing or DNA editing, allows a gene to be added, removed or altered at a precise location in the human genome.
If everything goes as planned, genetic edits will eliminate the root cause of genetic disorders.
There are more than 6,000 genetic disorders that are passed down from generation to generation. Ideally, gene editing technologies will generate treatments or cures for many of these disorders.
Common gene editing techniques include CRISPR, Zinc Finger Nuclease and TALENS. Scientists have been tinkering with ZFN and TALENS for about 20 years. CRISPR is the relatively new version of genome editing. Scientists have been using CRISPR in laboratories for about 10 years.
In 2020, a small handful of gene editing therapies are beginning to enter into human clinical trials. This is exciting, as we now get our first glimpse of data that indicates how safe and effective genome editing is when applied to humans.
A recent March 2020 paper published in Science demonstrates that patients’ immune cells (T-cells) can be genetically modified with CRISPR and then infused back into cancer patients with the intention of reducing cancer burden. Early data suggests this process was safe and the human cells were successfully modified. I’ll provide more insight into this clinical trial at the bottom of the page.
Below, I’ve built a table that lists and briefly describes ongoing human trials that rely on genome editing technologies. My intention is to keep a broad audience up to date on the future potential of gene editing.
I’ll update the table every 6 months.
Table 1. Human clinical trials based on gene editing technology (updated 2020)
Disease |
Group in pursuit (strategy) |
|---|---|
| Cancer (PD-1 knockout) | Hangzhou Cancer Hospital
Sichuan University
U Penn/Parker Institute |
| Cancer (multiple myeloma) | CRISPR Therapeutics
|
| Cancer (lymphoma) | CRISPR Therapeutics
|
| Hemoglobinopathies (β-thalassemia, sickle cell disease) | Vertex Pharmaceutical/CRISPR Therapeutics |
| Hemophilia B | Sangamo
|
| HIV | Affiliated Hospital to Academy of Military Medical Sciences
Sangamo
|
| Leber congenital amaurosis 10 (LCA10)
(hereditary blindness) |
Allergan/Editas |
| MPS I (Hurler syndrome) | Sangamo
|
| MPS II (Hunter’s syndrome) | Sangamo
|
ZFN: zinc finger nuclease
CRISPR: clusters of regularly inter-spaced short palindromic repeats, learn more about biology of CRISPR.
The table above lists human trials in significant phases of the approved drug pipeline. Other genome editing projects are ongoing but they’re at an earlier stage. Did I leave out a gene editing trial? Please let me know and I’ll update the table. Thanks!
More information on the 2020 Science paper on CRISPR human clinical trials
Three patients with advanced cancer are the first US humans to be treated with CRISPR technology. Carl June is the lead author on this project. In March, 2020, Dr. June and colleagues published an update on the patient’s condition. Before the CRISPR treatment, all three patients had been heavily pre-treated with chemotherapy. These were late stage cancer patients with a high likelihood of death. One patient has already died, while the other two have seen their cancer progress. However, the focus of this early project was to test the safety of delivering gene edited cells into human. In that regard, this project is deemed a success.
“These patients had no other treatment options left,” said Carl June, MD, director of the Center for Cellular Immunotherapies at the Perelman School of Medicine at the University of Pennsylvania and senior author of the paper. “The study wasn’t designed to test for efficacy — this was just a safety and feasibility study. For example, we wanted to know if the therapy would work at all in such heavily pretreated patients,” he added.
T-cells were first removed from the patient’s blood. Once moved to a laboratory, scientists applied CRISPR-CAS-9 tools to the cells to deliver gene edits. Once modified, these T cells were then infused back into the patient’s blood with an IV infusion.
The scientists removed two genes (TCR and PD-1) from the patient’s T cells. The idea is that by removing these genes, the T cells will remain aggressive and persist in the body for a longer amount of time. This seems to have worked. The modified T cells were found to persist for 9 months and were located in the tumor region of the body. This group also inserted a synthetic, cancer specific TCR transgene (NY-ESO-1) into the T cells. This TCR should allow these cells to track down and kill tumor cells.
The modified T cells also showed persistence and trafficking to the tumor sites, giving hope that these modifications introduced by the gene editing may help tackle the T-cell exhaustion that is often seen when treating solid tumors with chimeric antigen receptor T cells (CAR-T). ~ Cancer Therapy Advisor
Important note regarding the human modification:
All of the trials above involve somatic cell gene editing in humans. That means the genetic change is delivered to a part of the body that will not contribute to the sperm or egg cells. This is important because it means these genetic changes will not modify the patient’s children. In order to alter the downstream lineage (children) of these patients, you need to perform genetic edits in the patients’ germ cells. Germ cells include: sperm, egg and embryos. In 2018, a Chinese doctor named He Jiankui received a lot of bad press because he applied CRISPR to germ cells during a human experiment.
There are currently no human gene editing trials in the United States that involve delivering edits to germ cells. Well, at least none that I’m aware of…
How is gene therapy different than gene editing?
Gene therapy delivers a new gene into cells to compensate for a defective gene. However, gene therapy doesn’t remove or modify the defective DNA from a patients’ cells.
In contrast, genome editing removes or modifies the defective DNA in its native location within the genome. Most gene therapies use viral vectors to randomly insert a gene into a chromosome or else into an extra-chromosomal exosome.
Genome editing strategies rely on different types of strategies to deliver CRISPR into cells. Viral vectors are one of these strategies.
If interested, I’ve created this gene therapy page, which includes a table of active human clinical trials.